New data are available from the U.S. Census Bureau which provide estimates of the July 1, 2018 population for the nation, states, and counties by age, sex, race, and Hispanic origin. The latest brief from the Pennsylvania State Data Center highlights statewide trends in Pennsylvania’s changing population. As of 2018, Pennsylvania’s fastest growing populations include the population age 65 and over, the Hispanic or Latino population, and the non-Hispanic Asian population. Click here to read more.
Report: Pennsylvania employment strong, but job growth leaves regions, industries behind
UNIVERSITY PARK, Pa. — With the U.S. economy on track for potentially the longest expansion on record after the Great Recession of 2008-09, employment in Pennsylvania overall is strong. But the rosy statewide job numbers can mask persistent decline in various industries and regions across the state, according to economists in Penn State’s College of Agricultural Sciences.
Their conclusions are reflected in a report newly released by Penn State’s Center for Economic and Community Development, titled “Pennsylvania: Bust to Boom? Great Recession to Recovery & Beyond.” Through the liberal use of graphics, the report illustrates job growth and decline statewide and in five regions and 20 major industry sectors.
“While the Pennsylvania economy as a whole shows strength, it’s important to look at the distribution across the state,” said co-author Theodore Alter, professor of agricultural, environmental, and regional economics and the center’s co-director. “There’s a diversity of impact, and looking at the aggregate doesn’t give the correct picture.”
The report’s findings mirror those of two companion reports on the geography of employment and population shifts — released by the center in 2018 and earlier this year, respectively — that showed a significant contrast between southeastern Pennsylvania, which enjoyed mainly job and population growth from 2000 to 2017, and the rest of the state, with primarily declines.
The trends woven through this trilogy of reports suggest the existence of “two Pennsylvanians,” noted co-author Theodore Fuller, development economist in the Department of Agricultural Economics, Sociology and Education.
“Employment change in Pennsylvania’s five regions over the 10 years [2008-2018] covered in this report ranged from solid growth in southeastern Pennsylvania to widespread decline in western counties, and a mix of growth and decline in central, northern and northeastern Pennsylvania,” Fuller said. “This pattern was most stark during the recession and recovery but continued into the post-recovery growth years of 2015 to 2018.”
As an example, he pointed out that the 15 counties designated as southeastern Pennsylvania gained 133,000 jobs from 2015 to 2018, with 80,000 of that increase coming in the five-county Philadelphia metropolitan statistical area. In contrast, the 19-county western region gained only 3,000 jobs. While employment increased by 16,000 in the seven-county Pittsburgh MSA during this period, the other western counties combined lost a net of 13,000 jobs.
Fuller added that two major industrial developments underway that soon could bolster job creation and stimulate the economy of western Pennsylvania are construction by Royal Dutch Shell of a natural gas “cracker” plant in Beaver County — expected to be operational in the early 2020s — and a $1 billion investment by U.S. Steel to upgrade its Mon Valley Works by 2022.
In addition to regional changes in employment, there were winners and losers among industries, the report showed. Manufacturing and retail trade were in the top three industries in total employment in 2018, but they lost, by far, the most jobs among the 20 major sectors between 2008 and 2018. Manufacturing employment fell by nearly 80,000 and retail trade jobs declined by more than 28,000 over the 10-year period. Other industries with significant job losses were wholesale trade and educational services.
On the other hand, the state’s largest employment sector, health care and social services, gained more than 165,000 jobs during 2008-2018. In 2018, almost one in five Pennsylvanians was employed in this sector. Other growth industries included accommodation and food services, transportation and warehousing, and professional and technical services.
Pennsylvania’s top employment sector, health care and social services, gained 165,000 jobs in the 10-year period ending in 2018, but the largest number of those jobs were categorized as low-wage positions.
However, employment change doesn’t tell the whole story, the researchers said. Examining the average weekly wages of the jobs gained and lost provides additional insight. For instance, of all the jobs added in health care and social services between 2008 and 2018, by far the largest number were categorized as low-wage positions.
Across all the sectors analyzed, the greatest growth was in low-wage jobs, and the greatest losses came in middle-wage jobs, fueled by the decline in manufacturing employment. “Since 2008, we’ve seen a hollowing out of that middle-wage area,” Alter said. “And that suggests widening inequality, which could have profound implications for Pennsylvania’s economy going forward.”
The report is available on the Center for Economic and Community Development website.
Other contributors to this report were undergraduate research associates Raymond Hoy, Nolan Martino and Tessa Sontheimer; and Cristy Halerz Schmidt, applied research educator, Center for Economic and Community Development, Penn State. The U.S. Department of Agriculture’s National Institute of Food and Agriculture supported this work.
New Resource: Management Methodologies and Value-Based Strategies: An Overview for Rural Health Care Leaders
The Rural Health Value team has released a new resource outlining eight commonly used change management methodologies that are rural-relevant. It is intended as a guide to help rural health care leaders identify which approach(es) might be most useful to them and their organizations.
Management Methodologies and Value-Based Strategies: An Overview for Rural Health Care Leaders – Offers rural health leaders an overview of eight commonly used management methodologies to help guide change, plus additional resources and references for further exploration. (June 2019)
Top resources on the Rural Health Value website:
- Value-Based Care Assessment – Assess capacity and capabilities to deliver value-based care. Receive an eight category readiness report.
- Physician Engagement – Score current engagement and build effective relationships to create a shared vision for a successful future.
- Board and Community Engagement – Hold value-based care discussions as part of strategic planning and performance measurement.
- Social Determinants of Health – Learn and encourage rural leaders/care teams to address issues to improve their community’s health.
Contact information:
Keith J. Mueller, Ph.D.
Co-Principal Investigator
Unmet Need for Personal Care Assistance Among Rural and Urban Older Adults
Unmet Need for Personal Care Assistance Among Rural and Urban Older Adults. Despite differences in health, health services, economic, and demographic characteristics, little is known about whether rural and urban areas differ in unmet need for personal care for older adults with functional limitations. This brief from the University of Minnesota Rural Health Research Center addresses that gap by analyzing rural-urban differences in unmet need for help across 11 activities
Commonwealth Fund Releases 2019 Scorecard on State Health System Performance
(June 12, 2019) The Commonwealth Fund’s 2019 Scorecard on State Health System Performance reveals that most states are losing ground on key measures related to life expectancy as premature deaths from suicide, alcohol, and drug overdose continue to increase. Several states that most recently expanded eligibility for their Medicaid programs saw meaningful gains in access to health care; in other states prior gains eroded between 2016 and 2017. Finally, the Scorecard found that health care costs are placing an increasing financial burden on families across the nation.
In addition, you can download the full report, and a two-page summary for each state.
Child Diversity in Pennsylvania, 2009 to 2017
This research brief from the Pennsylvania State Data Center, Child Diversity in Pennsylvania, examines trends in the changing racial and ethnic makeup of Pennsylvania’s child population. The brief accompanies an interactive visualization which shows trends in race and ethnicity by school district and age group for those under 20 years.
The report shows that nearly a third of all children in Pennsylvania are children of color as of 2017, up from a quarter in 2009. Meanwhile, just one in five adults are persons of color. Four out of five school districts had higher shares of children of color in 2017 than 2009. Click here to read more in the full report, or click here to go straight to the visualization.
The report and visualization were developed in collaboration with our affiliate, Pennsylvania Partnerships for Children. Learn more about their important work at https://www.papartnerships.org/.
The Impact of Food Assistance on County-Level Employment
The Economic Research Service (ERS) at the U.S. Department of Agriculture (USDA) recently released a study on the economic impact of the Supplemental Nutrition Assistance Program, also known as SNAP. According to their research, consumers’ use of SNAP benefits had a greater impact in rural areas during national economic downturn, creating additional jobs in those counties. The ERS conducts research and analysis on a broad range of economic and policy topics related to agriculture and rural areas. The report can be accessed here: https://www.ers.usda.gov/publications/pub-details/?pubid=93168.
Study Ties Poor Oral Health in Kids to Adult Heart Disease Risk
Reuters Health reports on a new study that finds children who develop cavities and gum disease may be more likely to develop risk factors for heart attacks and strokes decades later than kids who have good oral health. Kids who had even one sign of poor oral health were 87% more likely to develop subclinical atherosclerosis; children with four signs of poor oral health were 95% more likely to develop this type of artery damage. Periodontal disease in adults has long been linked to increased risk of cardiovascular disease.
New Report Details Broadband Access Across Pennsylvania
A new report has been released, Broadband Availability and Access in Rural Pennsylvania. The project, funded by the Center for Rural Pennsylvania and conducted by researchers at Penn State, details broadband access across Pennsylvania and makes policy recommendations for the General Assembly to address broadband access disparities.
According to the report, over 800,000 Pennsylvania residents do not have access to broadband connectivity, according to the Federal Communications Commission (FCC). However, recent research has documented that these official estimates are downplaying the true state of the digital divide because they rely on self-reported data by Internet Service Providers (ISPs). Informed policy requires systematic analysis to both verify the FCC’s numbers and accurately determine the true state of broadband connectivity across Pennsylvania. The research collected more than 11 million broadband speed tests from across Pennsylvania in 2018. These tests measured broadband speeds in every Pennsylvania county and found that median speeds across most areas of the state do not meet the FCC’s criteria to qualify as broadband. The main findings from these analyses have profound implications for existing and future efforts to bridge the digital divide.
The full report can be accessed on the Center for Rural Pennsylvania’s website at https://www.rural.palegislature.us/
New Pre-K for Pennsylvania Report Released This Week
 New Pre-K for PA Report Released This Week
New Pre-K for PA Report Released This Week
This week the Pre-K for PA Campaign released a report, Ready to Succeed: Kindergarten Teachers Support Investments in High-Quality Pre-k, based on findings of a survey conducted with campaign partner PSEA. The results show resounding support for high-quality pre-k among those surveyed.
PPC President and CEO Kari King joined fellow campaign members at an event at Hamilton Elementary School in the Carlisle Area School District in Cumberland County to release the report, noting, “Investments in high-quality pre-k have a significant return on investment for our children, schools and communities. However, the state is not investing enough to ensure access for the children who need it the most.”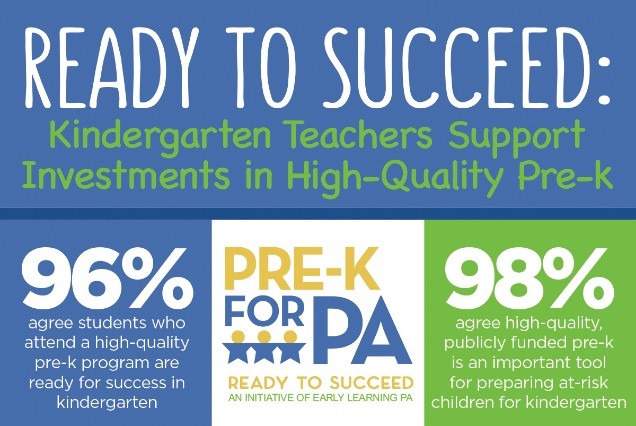
More than 97,000 – or 56 percent – of eligible 3- and 4-year-olds do not have access. The Pre-K for PA Campaign is calling for a $50 million increase in the 2019-20 state budget; $40 million for Pre-K Counts and $10 million for the Head Start Supplemental Assistance Program (HSSAP). This investment will provide access to an additional 5,500 children.
