- CMS: Medicare Program; Implementation of Prior Authorization for Select Services for the Wasteful and Inappropriate Services Reduction (WISeR) Model
- Public Inspection: CMS: Medicare Program: Implementation of Prior Authorization for Select Services for the Wasteful and Inappropriate Services Reduction Model
- CMS: Secretarial Comments on the CBE's (Battelle Memorial Institute) 2024 Activities: Report to Congress and the Secretary of the Department of Health and Human Services
- HHS: Patient Protection and Affordable Care Act: Marketplace Integrity and Affordability
- HRSA Announces Action to Lower Out-of-Pocket Costs for Life-Saving Medications at Health Centers Nationwide
- Public Inspection: HHS: Patient Protection and Affordable Care Act: Marketplace Integrity and Affordability
- Increased Risk of Cyber Threats Against Healthcare and Public Health Sector
- Eight Hospitals Selected for First Cohort of Rural Hospital Stabilization Program
- Announcing the 2030 Census Disclosure Avoidance Research Program
- CMS: Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Policy Changes and Fiscal Year 2026 Rates; Requirements for Quality Programs; and Other Policy Changes; Correction
- CMS: Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Policy Changes and Fiscal Year 2026 Rates; Requirements for Quality Programs; and Other Policy Changes; Correction
- CMS: Medicare and Medicaid Programs; Contract Year 2026 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly; Correction
- CMS: Medicare and Medicaid Programs; Contract Year 2026 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly; Correction
- CMS: Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities; Updates to the Quality Reporting Program for Federal Fiscal Year 2026
- CMS: Medicare Program; FY 2026 Hospice Wage Index and Payment Rate Update and Hospice Quality Reporting Program Requirements
New Pre-K for Pennsylvania Report Released This Week
 New Pre-K for PA Report Released This Week
New Pre-K for PA Report Released This Week
This week the Pre-K for PA Campaign released a report, Ready to Succeed: Kindergarten Teachers Support Investments in High-Quality Pre-k, based on findings of a survey conducted with campaign partner PSEA. The results show resounding support for high-quality pre-k among those surveyed.
PPC President and CEO Kari King joined fellow campaign members at an event at Hamilton Elementary School in the Carlisle Area School District in Cumberland County to release the report, noting, “Investments in high-quality pre-k have a significant return on investment for our children, schools and communities. However, the state is not investing enough to ensure access for the children who need it the most.”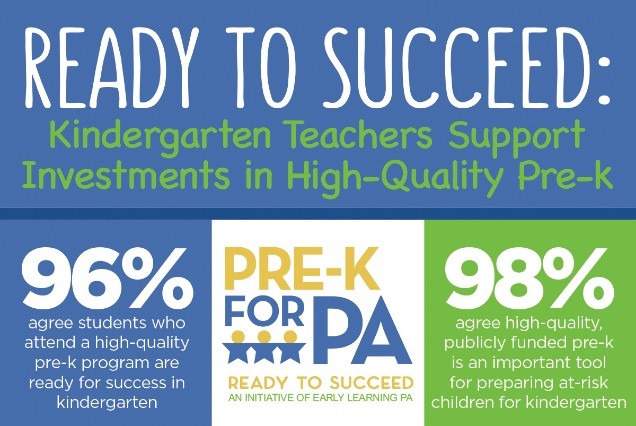
More than 97,000 – or 56 percent – of eligible 3- and 4-year-olds do not have access. The Pre-K for PA Campaign is calling for a $50 million increase in the 2019-20 state budget; $40 million for Pre-K Counts and $10 million for the Head Start Supplemental Assistance Program (HSSAP). This investment will provide access to an additional 5,500 children.
Improving Oral Health Care Services in Rural America
Improving Oral Health Care Services in Rural America. The shortage of practicing dental professionals in rural communities is influenced by a variety of factors, especially the limited number of dentists who are able and/or willing to start a rural practice. The archive of this hour-long presentation is now available, in which experts discuss policy recommendations in the recent report on this topic from the National Advisory Committee on Rural Health and Human Services.
Health Professions Training Programs Dashboard
Health Professions Training Programs Dashboard. Visit HRSA’s new dashboard at data.HRSA.gov to view data from HRSA’s Bureau of Health Workforce education and training programs for academic year 2012–2013 to present. Find out how these health workforce grant programs are supporting HRSA’s goal of providing high quality, culturally competent care in rural and underserved communities.
Supporting Rural Health: Practical Solutions for State Policymakers
Supporting Rural Health: Practical Solutions for State Policymakers. With input from HRSA’s Federal Office of Rural Health Policy, the Milbank Memorial Fund presents this issue brief with findings from three regional meetings of federal and state health officials and health services researchers working on rural issues. Case studies summarized in the brief shed light on successful models for incentivizing investment, the need for workforce development, and the need for ongoing research and policy development specifically directed toward rural health.

David B. Nash, MD, MBA, Founding Dean, Jefferson College of Population Health, has announced that the application process is now open for the 2020 Hearst Health Prize! The winner will receive a $100,000 prize in recognition of outstanding achievement in managing or improving population health. Up to two finalists will receive a cash award of $25,000 each.
The Hearst Health Prize, in partnership with the Jefferson College of Population Health (JCPH), was created to help identify and promote promising initiatives in the field that improve health outcomes. The goal is to discover, support, and showcase the work of an individual, group, or institution that has successfully implemented a population health program that has made a measurable difference.
Last year, they received over 150 impressive submissions from across the country showcasing a range of projects aimed at improving the health of populations. The 2019 winner, Sharp Transitions, was recognized at the Population Health Colloquium for its outstanding home-based palliative care program for patients with advanced and progressive chronic illness who are not ready for hospice care. Additionally, two finalists, Arkansas SAVES, and Mental health Outreach for MotherS (MOMS) Partnership® were each awarded $25,000 for their impactful programs.
Finalists will be invited to present their project during a special poster session at the Population Health Colloquium in Philadelphia, March 30-April 1, 2020. The winner of the prize will be announced during the opening session of the Population Health Colloquium on March 31, 2020.
To apply or learn more about the Hearst Health Prize visit: Jefferson.edu/HearstHealthPrize. The deadline to submit an application is Friday, August 9, 2019, 3:00 PM (EDT)/12:00 Noon PM (PDT).
If you have any questions, please email HearstHealthPrize@Jefferson.edu. Please share this amazing opportunity with your colleagues!
Medicare Dental Benefit Act Introduced in House
Representative Nanette Diaz Barragan (D-CA) introduced the Medicare Dental Benefit Act of 2019, H.R. 2951 which, if passed, will add dental coverage to Part B of the Medicare program. The legislation has now been introduced in both chambers of Congress. This is another milestone in efforts to elevate the need for improved oral health coverage in public health care programs.
Briefs Published on Identifying High-Need Rural Counties to Help in Resource Location Planning
The Rural Minority and Minority Health Research Center at the University of South Carolina has published two policy briefs.
The first brief, Identification of High-Need Rural Counties to Assist in Resource Location Planning, categorizes high-need, low-resource locations by identifying counties that lacked safety-net providers.
The second brief, Identification of High-Need Rural Counties to Assist in Resource Location Planning for Primary Care, examines areas with poor health outcomes and limited access to primary care safety net settings.
Economic Impact of a Bad Smile Estimated at $27 Million
An article in the Journal of Public Health Dentistry describes the impact improving oral health could have on employability. Dr. Halasa-Rappel, PhD and her co-authors used the National Health and Nutritional Examination Survey to develop a Dental Problem Index (DPI) to quantify the impact of dental caries and missing anterior teeth on employment, and estimate the impact of a routine dental visit on the health of anterior teeth and the benefits of expanding dental coverage for non-elderly adults. They found that a routine dental visit has a negative impact on the DPI and improves the probability of employment and estimated that improvement in dental coverage would improve the employability of 9,972 non-elderly adults with an associated annual fiscal impact of $27 million.
NHSC Starts News Rural Loan Repayment Program
The National Health Service Corps (NHSC) Rural Community Loan Repayment Program (LRP) is a new program for providers working to combat the opioid epidemic in the nation’s rural communities. The application cycle will open soon and you can sign up for email notices. The NHSC LRP will make FY 2019 loan repayment awards in coordination with the Rural Communities Opioid Response Program (RCORP) initiative within the Federal Office of Rural Health Policy (FORHP) to provide evidence-based substance use treatment, assist in recovery, and to prevent overdose deaths across the nation. Check out information on the NHSC Rural Community Loan Repayment Program website.
Cost Inhibits Access to Care
More than 25% of rural U.S. residents had trouble accessing health care in the last few years, and almost half of them reported it was because they could not afford the care, according to a survey by NPR, the Robert Wood Johnson Foundation, and the Harvard T.H. Chan School of Public Health released this week. The survey found that 49% of respondents said they would not be able to afford an unexpected expense, such as a medical bill totaling $1,000. (Source: NPR’s “Shots,” 5/21)
