Secretary of the U.S. Department of Health & Human Services Alex Azar issued a statement this week about the outbreak of measles, now diagnosed in more than 700 cases across the country. The Centers for Disease Control and Prevention (CDC) has confirmed outbreaks in 22 states. Symptoms of measles generally appear about seven to 14 days after a person is infected and typically include high fever, cough, runny nose, and a rash of flat, red spots. Available data do not indicate that rural areas are more or less affected, but the CDC’s national surveys that monitor vaccination coverage have identified that unvaccinated children are more likely to be uninsured, live below the poverty level, and live in rural areas. Many may not know about the CDC’s Vaccines for Children Program that serves children up to age 18 who are uninsured or underinsured, or who receive care through Federally Qualified Health Centers or Rural Health Clinics. Adults who are unsure of their measles vaccination status should consider getting the updated Measles Mumps Rubella (MMR) vaccine.
Pennsylvania Substance Use Disorder Loan Repayment Program Practitioner Application Announced
May 1, 2019
Applications are invited to the Pennsylvania Department of Health’s Pennsylvania Substance Use Disorder Loan Repayment Practitioner Program, in accordance with RFA # 67-86.
All questions regarding this RFA must be directed in writing by e-mail to RA-DHSUDLRP@pa.gov, no later than May 12, 2019. All questions must include the specific section of the RFA about which the potential applicant is questioning. Answers to all questions will be posted at https://www.health.pa.gov/topics/Health-Planning/Pages/SUD-LRP.aspx on or before May 17, 2019.
Please submit an application via the on-line Pennsylvania Substance Use Disorder Loan Repayment Program Practitioner Application found at the following website: https://www.health.pa.gov/topics/HealthPlanning/Pages/SUD-LRP.aspx, beginning Wednesday, May 1, 2019. Completed applications must be submitted before 11:59 p.m. on Monday, June 3, 2019.
LATE APPLICATIONS WILL NOT BE ACCEPTED REGARDLESS OF THE REASON.
It is expected that the evaluation of applications and the selection of grantees will be completed within six weeks of the submission due date.
USDA Releases Report on Rural Broadband and Benefits of Next Generation Precision Agriculture
Reliable, High-Speed Broadband e-Connectivity is Essential to Enhanced Agricultural Production
WASHINGTON, April 30, 2019 – Agriculture Secretary Sonny Perdue today unveiled a groundbreaking report, A Case for Rural Broadband: Insights on Rural Broadband Infrastructure and Next Generation Precision Agriculture Technologies (PDF, 2.5 MB). The report finds that deployment of both broadband e-Connectivity and Next Generation Precision Agriculture Technology on farms and ranches throughout the U.S. could result in at least $47 billion in national economic benefits every year.
“Broadband and Next Generation Precision Agriculture are critical components for creating vital access to world-class resources, tools and opportunity for America’s farmers, ranchers, foresters and producers,” Secretary Perdue said. “Under the leadership of President Trump, USDA is committed to doing our part to clear the way for nationwide broadband connectivity that will allow the next generation of precision agriculture technologies to thrive and expand.”
Download A Case for Rural Broadband: Insights on Rural Broadband Infrastructure and Next Generation Precision Agriculture Technologies (PDF, 2.5 MB). To see how Next Generation Precision Agriculture Technologies can work on farm and ranching operations, view the Connected Technologies infographic (PDF, 910 KB).
The report also finds that if broadband infrastructure and digital technologies at scale were available at a level that meets estimated producer demand, the U.S. economy could realize benefits equivalent to nearly 18 percent of total agriculture production. Of that 18 percent, more than one-third is dependent on broadband e-Connectivity, equivalent to at least $18 billion in annual economic benefits that only high-speed, reliable internet can provide.
For many years, USDA and the American agriculture industry have been actively researching the feasibility, usage and potential upside of Next Generation Precision Agriculture technologies. Until now though, the interdependency of these technologies and broadband e-Connectivity has not been evaluated. The report released today explores this symbiotic relationship and quantifies the potential economic benefit of broadband buildout and the complementary adoption of connected agriculture technologies. Going forward, the U.S. Department of Agriculture (USDA) will be engaged in multiple facets of infrastructure and technology deployment, including financing rural capital investments and supporting producers who are exploring which Next Generation Precision Agriculture Technologies are best suited to improve their operations and serve their customers.
In April 2017, President Trump established the Interagency Task Force on Agriculture and Rural Prosperity to identify legislative, regulatory and policy changes that could promote agriculture and prosperity in rural communities. In January 2018, Secretary Perdue presented the Task Force’s findings to President Trump. These findings included 31 recommendations to align the federal government with state, local and tribal governments to take advantage of opportunities that exist in rural America. The Report identified Achieving e-Connectivity in Rural America as a cornerstone recommendation. The Administration has been executing this priority call to action through the American Broadband Initiative (ABI) (PDF, 647 KB), which reflects rural broadband build-out as one of President Trump’s directives to the Federal government. A Case for Rural Broadband: Insights on Rural Broadband Infrastructure and Next Generation Precision Agriculture Technologies (PDF, 2.5 MB) opens the next chapter in the USDA’s response to this call to action.
To view the report in its entirety, please view the Report to the President of the United States from the Task Force on Agriculture and Rural Prosperity (PDF, 5.4 MB). In addition, to view the categories of the recommendations, please view the Rural Prosperity infographic (PDF, 190 KB).
Information Released on the 2020 U.S. Census Impact on Services
The 2020 Census is closer than you think. The United States Census Bureau has released a public facing flyer detailing what the census is and why it is essential that everyone is counted, especially for services. Many large federal programs distribute funds based on population. Consider sharing the flyer in public places to encourage census participation.
Pennsylvania Oral Health Surveillance Plan Announced
The Pennsylvania Department of Health Oral Health Program is excited to announce the publication of the 2019-2024 Pennsylvania Oral Health Surveillance Plan. The Oral Health Surveillance Plan provides a consistent source of reliable and valid information for use in the monitoring of oral health status and trends of the state and for developing, implementing, and evaluating programs to improve the oral health of Pennsylvanians.
Congressional Budget Office Releases Report on Single-Payer Health Care System
Key Design Components and Considerations for Establishing a Single-Payer Health Care System
Congressional interest in substantially increasing the number of people who have health insurance has grown in recent years. Some Members of Congress have proposed establishing a single-payer health care system to achieve universal health insurance coverage. In this report, CBO describes the primary features of single-payer systems, as well as some of the key considerations for designing such a system in the United Stat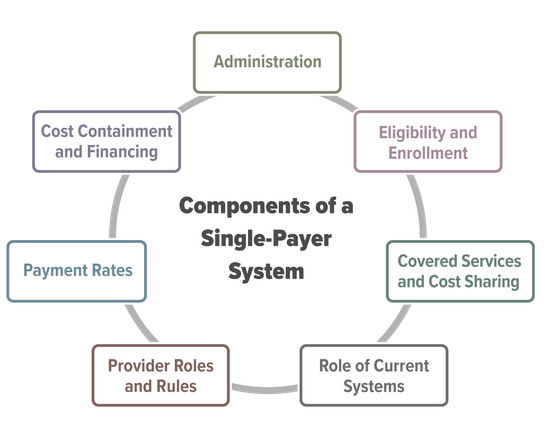 es.
es.
Establishing a single-payer system would be a major undertaking that would involve substantial changes in the sources and extent of coverage, provider payment rates, and financing methods of health care in the United States. This report does not address all of the issues that the complex task of designing, implementing, and transitioning to a single-payer system would entail, nor does it analyze the budgetary effects of any specific bill or proposal.
Primary Care Clinician Participation in the CMS Quality Payment Program
Clinton MacKinney, MD, MS; Fred Ullrich, BA; and Keith J. Mueller, PhD
Approximately 10 percent of primary care clinicians participate in Advanced Alternative Payment Models (A-APMs) and less than 30 percent of primary care clinicians participate in the Merit-Based Incentive Payment System. Metropolitan primary care clinicians are more likely to participate in A-APMs than non-metropolitan primary care clinicians.
Click to download a copy: Primary Care Clinician Participation in the CMS Quality Payment Program
Open Comment Period for Pennsylvania WIC
The Pennsylvania Women, Infants, and Children (WIC) program is accepting public comments on its program. Please consider mentioning the importance of oral health in WIC programming. Comments can be provided at upcoming WIC Public Meetings. Written comments can be sent via email to bmellott@pa.gov or mailed to The Department of Health, Bureau of Women, Children, Infants and Children (WIC), 625 Forster St., 7 West, Health and Welfare Building, Harrisburg, PA 17120. Written comments should be received by May 31.
Can we heal rural health? All eyes are on Pennsylvania’s bold experiment | Opinion
By Rachel Levine and Andy Carter, For the Philadelphia Inquirer, April 26, 2019
Rural communities and their hospitals are struggling.
In terms of health and well-being, rural Pennsylvania and urban Philadelphia have all too much in common, including high rates of child poverty and mortality, food insecurity, and chronic disease.
In terms of the health care needed to address these issues, rural hospitals face some unique challenges. These include sustaining a wide array of services for smaller numbers of patients due to sparsely populated geographies. About half of Pennsylvania’s rural hospitals operate at a loss and are at risk for closure.
Respected research organizations have reported on this problem nationwide. Since 2010, 104 U.S. rural hospitals have closed, two of them in Pennsylvania.
Pennsylvania’s bold experiment
In partnership with the Center for Medicare & Medicaid Innovation, the Pennsylvania Department of Health’s new Rural Health Model flips the script on hospital care. In place of hospitals’ traditional focus — treating patients when they are sick or injured — the new model also aims to reward hospitals for keeping patients healthy and out of the hospital altogether.
To accomplish these goals, the model changes the way hospitals are paid.
Typically, hospitals receive payment for each health care service they provide. With the Rural Health Model, hospitals get paid based on annual budgets, which provides more consistent cash flow. These budgets define the financial resources hospitals will have during the year — independent of how many patients are hospitalized or come to emergency rooms. Insurers (commercial and Medicare) and hospitals work together to establish budgets based on the payments hospitals typically received in the past.
With their financial footings a bit more predictable, hospitals can redirect resources and invest in services and partnerships to improve community health. Hospitals are encouraged to focus on keeping people healthy.
This new payment approach not only provides a measure of stability for hospitals, but also for rural communities and jobs.
In metropolitan areas, with a pick of health care systems and services, it may be hard to imagine how important a hospital is to its rural community. In emergencies, that hospital may be the only source of care for 20 miles or more.
Hospitalizations in rural Pennsylvania, across the state, and nationwide are going down.
Hospitals and health systems are shifting care to outpatient and home settings whenever safe and appropriate. Doctors, nurses, and health educators are working with patients, encouraging them to seek preventive care and improve health habits. The goal is to foster better quality of life and avoid intensive and costly inpatient care.
The Rural Health Model gives hospitals predictable finances — those annual budgets — and, potentially, additional flexibility with which to foster this move to better health and lower health care spending.
Now, instead of focusing on expanding services just for the sake of growing market share under the traditional fee-for-service model, hospitals can focus on providing the services most needed by the community. This right-sizing frees up resources to focus on the services needed to address the community’s biggest health challenges (diabetes, for example) and to kick start the virtuous cycle of better health and less need for hospital care.
Five Pennsylvania hospitals have signed up to test out this new payment strategy. (Five insurers have also joined the pilot.) The hospitals have defined strategies for how they will move from just providing sick care to also helping improve the overall health of their communities. Common strategies include better care coordination for patients with chronic disease and better geriatric care for older adults, with the goal of reducing expensive emergency room visits.
The pressing need to help rural communities become healthier, and the potential for this model, has attracted interest from scores of state and federal government agencies and health policy organizations. They really want to make this model work, and effective collaboration is key.
Creating the Rural Health Redesign Center would establish the hub to bring these resources together, to help with the planning and analysis needed to identify successful strategies and replicate them. Five hospitals are using the model now, and we have high interest from up to 25 additional hospitals in joining them over the next two years. Learning from one another about what works and what doesn’t will speed progress.
State legislation is needed to set up the Rural Health Redesign Center. Senate Bill 314, sponsored by Senator Lisa Baker, and House Bill 248, sponsored by Representative Tina Pickett, both have bipartisan support.
Governments, health departments, and hospitals across the nation are watching Pennsylvania’s experiment carefully. Since starting work on this model several years ago, we’ve heard from over a dozen different states, all asking: “Is it working?”
We invite you to pay close attention as well, and to learn more about how five hospitals and insurers are working together, exploring a new and better way to care for their communities. Pennsylvania’s Rural Health Model could help to usher in a new era of health care.
Rachel Levine, MD is Pennsylvania Secretary of Health. Andy Carter is president and CEO of the Hospital and Healthsystem Association of Pennsylvania.
Final Rule Announced Health Insurance Benefit and Payment Parameters
Last week, the Centers for Medicare & Medicaid Services (CMS) released the final Notice of Benefit and Payment Parameters for the 2020 benefit year, a document that sets forth instructions to insurers participating in the Health Insurance Exchanges or “Marketplaces”. Among the changes for 2020 are flexibilities related to the duties and training requirements for the Navigator program and opportunities for innovations in the direct enrollment process. In 2018 and 2019, the percentage of enrollments in the federal exchange (healthcare.gov) by rural residents remained unchanged at 18 percent.
