- CMS: Medicare Program; Implementation of Prior Authorization for Select Services for the Wasteful and Inappropriate Services Reduction (WISeR) Model
- Public Inspection: CMS: Medicare Program: Implementation of Prior Authorization for Select Services for the Wasteful and Inappropriate Services Reduction Model
- CMS: Secretarial Comments on the CBE's (Battelle Memorial Institute) 2024 Activities: Report to Congress and the Secretary of the Department of Health and Human Services
- HHS: Patient Protection and Affordable Care Act: Marketplace Integrity and Affordability
- HRSA Announces Action to Lower Out-of-Pocket Costs for Life-Saving Medications at Health Centers Nationwide
- Public Inspection: HHS: Patient Protection and Affordable Care Act: Marketplace Integrity and Affordability
- Increased Risk of Cyber Threats Against Healthcare and Public Health Sector
- Eight Hospitals Selected for First Cohort of Rural Hospital Stabilization Program
- Announcing the 2030 Census Disclosure Avoidance Research Program
- CMS: Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Policy Changes and Fiscal Year 2026 Rates; Requirements for Quality Programs; and Other Policy Changes; Correction
- CMS: Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Policy Changes and Fiscal Year 2026 Rates; Requirements for Quality Programs; and Other Policy Changes; Correction
- CMS: Medicare and Medicaid Programs; Contract Year 2026 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly; Correction
- CMS: Medicare and Medicaid Programs; Contract Year 2026 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly; Correction
- CMS: Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities; Updates to the Quality Reporting Program for Federal Fiscal Year 2026
- CMS: Medicare Program; FY 2026 Hospice Wage Index and Payment Rate Update and Hospice Quality Reporting Program Requirements
Final Recommendation Statement: Implementing Interventions to Prevent Falls in Community-Dwelling Older Adults

The U.S. Preventive Services Task Force released a final recommendation statement on interventions to prevent falls in community-dwelling older adults. The Task Force found that exercise can help prevent falls in adults 65 and older who are at increased risk. Additional interventions might be helpful for some older adults. To view the recommendation, the evidence on which it is based, and a summary for clinicians, please go here.
State Tobacco-Related Disparities Dashboard Released
 The state tobacco-related disparities dashboard, available on the Centers for Disease Control and Prevention (CDC) website, is an intuitive visualization platform. Use it to quickly explore cigarette smoking prevalence and related disparities in states by numerous factors. It can help you identify opportunities for improvement and action with your health center patients.
The state tobacco-related disparities dashboard, available on the Centers for Disease Control and Prevention (CDC) website, is an intuitive visualization platform. Use it to quickly explore cigarette smoking prevalence and related disparities in states by numerous factors. It can help you identify opportunities for improvement and action with your health center patients.
Register for HRSA Patient-Centered Medical Home Health Equity Symposium

Registration is now open for this annual symposium, which the Health Resources and Services Administration (HRSA) hosts in partnership with The Joint Commission. Join your peers and experts to hear about and discuss best practices and lessons learned in health equity, quality improvement, and accreditation and recognition. Visit the event to learn more and register for the Tuesday, July 16, and Wednesday, July 17, 12:00 – 4:00 pm symposium.
Text Reminders Help with Employee Burn Out
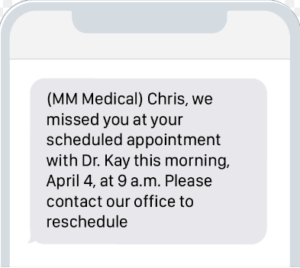
Healthcare workers everywhere are struggling with burn out, a problem that has only intensified since the COVID-19 pandemic. To combat burn out and improve employee mental health, institutions like Penn Medicine have adopted a mental health platform that sends regular, automated text messages connecting employees to resources specifically designed for healthcare workers. A recent study by JAMA Network Open showed that employees receiving text message reminders saw a dramatic improvement in their depression symptoms. Read more about the mental health platform and the study here.
Measure Impact in Recruitment Through Candidate Feedback
While there are many traditional ways of measuring your recruitment’s impact on your organization, candidate feedback is a tool that is often overlooked as an indicator of success. The information collected from candidates could provide crucial information for maximizing your recruitment strategy and improving processes. Check out this article to find out more.
Pennsylvania Distributes Funding to Dentists Providing Services to Medicaid Patients
 As part of the FY 2023-24 state budget, the Pennsylvania state legislature allocated $12 million to be used for the purpose of making one-time payments to dentists enrolled in the Medical Assistance (MA) program based on an enrolled dentist’s utilization from calendar year 2022 billing of 31 dental codes as compared to the total claims billed. Per the legislation, this program is only for dentists that submitted bills for the eligible services using Provider Type 27 (Dentist). That means that care provided by FQHC dentists is not eligible for this funding as FQHCs are enrolled as Provider Type 8 and the FQHC is both billing and rendering provider.
As part of the FY 2023-24 state budget, the Pennsylvania state legislature allocated $12 million to be used for the purpose of making one-time payments to dentists enrolled in the Medical Assistance (MA) program based on an enrolled dentist’s utilization from calendar year 2022 billing of 31 dental codes as compared to the total claims billed. Per the legislation, this program is only for dentists that submitted bills for the eligible services using Provider Type 27 (Dentist). That means that care provided by FQHC dentists is not eligible for this funding as FQHCs are enrolled as Provider Type 8 and the FQHC is both billing and rendering provider.
Employers Now Have Employee Health Insurance Coverage Options
Employers offering an Individual Coverage Health Reimbursement Arrangement (ICHRA) can reimburse employees with pretax dollars to cover the cost of individual health insurance premiums and qualified medical expenses. ICHRAs first became available in 2020, preceded by qualified small employer health reimbursement arrangements (HRAs) in 2017. Until then, the Affordable Care Act (ACA) prohibited employers from reimbursing employees for individual market premiums. Employers determine how much they will reimburse employees via an ICHRA health insurance plan. The same terms must apply to all workers within a given class, though reimbursements may be increased for older employees and those with more dependents. Some ICHRAs may be more affordable options because employers set how much they’re willing to spend and because they provide flexibility for employers who don’t or can’t offer healthcare insurance due to the cost. Unfortunately, not all employees can purchase individual coverage through marketplaces or receive premium tax credits. The coverage employers offer must not meet the Affordable Care Act Affordability standards and ensure enough employees participate or it may become cost prohibitive. Depending on the marketplace offerings, employers will have to determine if the risk or change is worth it.
Prime Pennie Contractor Acquired by Accenture Federal Services

Accenture Federal Services has completed its acquisition of Cognosante, a Falls Church, Virginia-based provider of digital transformation and cloud modernization solutions for federal health, defense, intelligence, and civilian agencies. Accenture Federal Services announced its intent to acquire Cognosante on April 15, 2024. Cognosante is the prime contractor under the current enrollment assistance contract for the Pennsylvania Health Insurance Exchange (Pennie). Founded in 2008 by Michele Kang, Cognosante has grown rapidly and is providing technology solutions to federal government clients, including healthcare programs supporting veterans, active-duty military, patients, beneficiaries, providers, and payors. Through CMS’s Center for Consumer Information and Insurance Oversight (CCIIO), Cognosante assisted with an Enrollment Assistance Program to ensure continuity of coverage for individuals and families impacted by the Medicaid Unwinding.
Pennsylvania House Insurance Committee Prepares to Vote on Senate-Passed Telemedicine Bill

The House Insurance Committee unanimously passed a telemedicine bill that passed the state Senate last month. Senate Bill 739 would require that health insurance policies cover medically necessary and otherwise covered healthcare services delivered through telemedicine. The bill was approved by the Senate by a 47-1 vote. The bill does allow telemedicine services to be provided by FQHCs. The bill now goes to the House for a vote. Since the bill was amended in the House Insurance Committee, it would need to go to the Senate for final approval.
New Strategic Plan for Aging in Pennsylvania Launched: Aging Our Way, PA
Pennsylvania Governor Josh Shapiro and the Department of Aging Secretary Jason Kavulich unveiled a new blueprint for enhancing services targeted at the state’s elderly population. The plan, “Aging Our Way, PA,” is a ten-year strategic plan aimed to transform how state, regional, and local agencies work together to meet the needs of Pennsylvania’s fast-growing senior population and improve their quality of life.
