- RPHARM Program Fulfills Need for Rural Pharmacists
- Farmers Don't Do Mental Health
- A Pilot Program in Rural Vermont Hopes to Build a Blueprint for Substance Abuse Recovery
- Rural Telehealth Extension Reintroduced in Congress
- Students From Across the State Emphasized the Need for Mental Health Resources in Rural Alaska During a Conference
- The South Was the Center of Rural Population Growth Last Year
- How HHS SUD Confidentiality Regulations Will Impact Rural Providers
- VA Announces Expansion of "Close to Me" Cancer Program as Part of the Cancer Moonshot, Bringing Cancer Diagnosis and Treatment Closer to Thousands of Veterans
- Navajo Psychiatrist Bridges Gaps Between Native American Culture and Behavioral Health Care
- Biden-Harris Administration Releases National Strategy for Suicide Prevention and First-Ever Federal Action Plan
- Biden-Harris Administration Takes Historic Action to Increase Access to Quality Care, and Support to Families and Care Workers
- Rural Communities Face Primary Care Physician Shortage
- Rural Jails Turn to Community Health Workers To Help the Newly Released Succeed
- Biden Administration Sets Higher Staffing Mandates. Most Nursing Homes Don't Meet Them.
- Miles for Milk: How Student-Run Grocery Store Reshaped Rural Community's Food Access
AJPH Call for Papers on Rural Public Health –
The American Journal of Public Health (AJPH) invites papers assessing the role of government policy in the status and revitalization of rural health. They seek papers that describe rural health research, report on interventions in rural settings, assess the impact of laws and policies, and examine the human health impact of climate change in rural areas. AJPH also invites editorials and commentaries proposing ways to apply public health methods that have been successful in other regions of the world, describing potential sources of funding, and depicting a vision for a rural public health of the 21st century. Potential authors should visit the AJPH website to review instructions for authors and specific guidelines for the various types of manuscript formats. Abstracts are due on January 15, 2020.
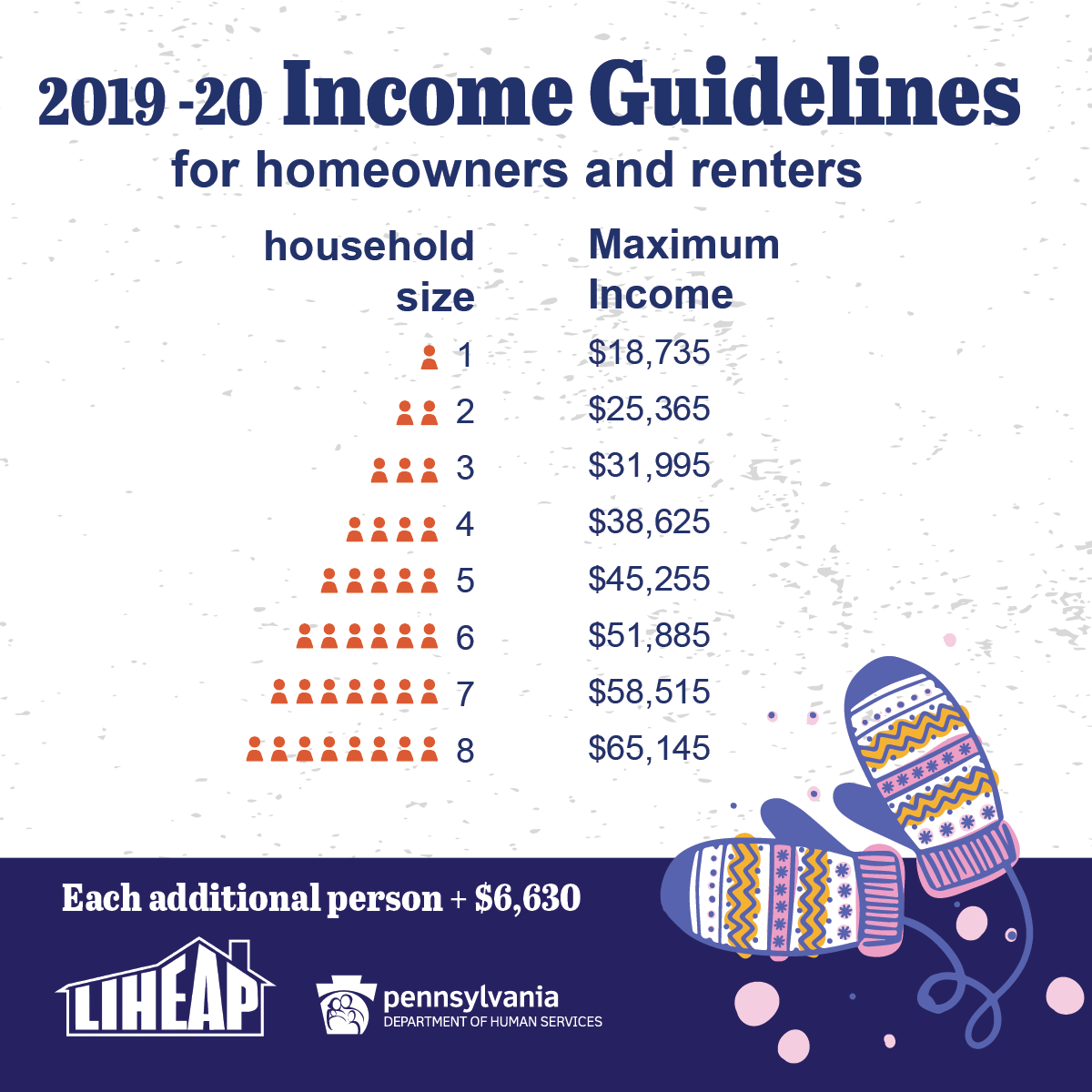
Home Heating Assistance is Now Available for Pennsylvania Families
LIHEAP, which stands for the Low-Income Home Energy Assistance Program, helps families living on low incomes pay their heating bills in the form of a cash grant. Crisis grants also are available for households in immediate danger of being without heat.
How cash grants work
A one-time payment is sent directly to the utility company/fuel provider and is credited on the heating bill. Cash grants range from $200 to $1,000 based on household size, income, heating region, and fuel type.
Qualifying crisis situations
- Broken heating equipment or leaking lines that must be fixed or replaced
- Lack of fuel
- Main heating source has been completely shut off
 Danger of being without fuel (less than 15-day supply)
Danger of being without fuel (less than 15-day supply) - Danger of having utility service terminated (received a notice that service will be shut off within the next 60 days)
Eligibility
- There are income guidelines.
- Applicants do not have to be on public assistance.
- Applicants don’t need to have an unpaid heating bill.
- Applicants can rent or own their home.
What’s needed to apply?
- Names of people in the household
- Dates of birth for all household members
- Social Security numbers for all household members
- Proof of income for all household members
- Recent heating bill or delivery receipt from the previous year
[For crisis situations, a person may need a copy of the shut-off notice.]
How to apply
Pennsylvanians can apply for LIHEAP three ways: online, on paper, and in person.
Online
Apply for LIHEAP benefits online using COMPASS. New this year: Those who received LIHEAP last year can apply for home-heating assistance via the mobile app, myCOMPASS PA. They’ll need the preseason application or green postcard we sent via mail to apply on the app.
On paper
Pennsylvanians can download an English or Spanish version of the application, fill it out, and return it to their county assistance office.
In person
Pennsylvanians can visit their county assistance office for help filling out the application in person. Applications also are available at senior centers and other community agencies.
Contact us for help
For more information about LIHEAP, Pennsylvanians can call the LIHEAP hotline at 1-866-857-7095, or can contact their county assistance office, Monday through Friday. Individuals with hearing impairments may call 711.
Visit the website
Find all of this information and more on the DHS website. View the state plan for LIHEAP and download brochures to print and share.
Forbes Explains How Urbanization Exacerbates the Health Care Crises in Rural America
Forbes reports that according to the USDA’s Economic Research Service, between 2010 and 2017, almost 1,000 rural counties in the U.S. recorded more deaths than births. Simultaneously, rural populations have declined, with only 20% of the population residing in rural areas which make up 97% of the country. Population change also means significant changes in health care need, demand and access. Also, according to the National Institute for Health Care Management (NIHCM), “As urbanization increases, an older, sicker and poorer population remains in rural America.” What this means is that Americans living in rural areas of the country have much greater health issues, and far fewer health resources.
Support for the Rural ACO Improvement Act Builds
The Rural ACO Improvement Act (S.2648) is gaining momentum on Capitol Hill. The recently introduced Senate bill would revise the Medicare Shared Savings Program benchmarking process and level the playing field for rural accountable care organizations. NRHA supports and applauds the legislation as a critical step to ensure all providers, regardless of zip code, are able to benefit from the program. We are proud that other associations with vested interested in the future of rural health care, such as AAFP, are joining us in supporting this meaningful rural health legislation.
Several Hospital Associations in Rural States Support a Senate Finance Rural Health Package
Rural hospital leaders nationwide are urging lawmakers to respond to the rural health care crisis. As rural hospitals are left with tough choices, like shutting down their obstetric unit, policy changes are necessary. New reporting claims that several state hospital associations are in support Congress enacting legislative fixes to ensure the sustainability of rural hospitals. The various state hospital associations support a rural health package with NRHA-backed solutions, such as allowing struggling rural PPS hospitals to convert to CAHs, and a long-term solution of a new payment model. We look forward to working alongside these associations as we urge Congress to act.
NRHA Appropriations Watch Update
During the week of October 28, 2019, the Senate appropriators passed their four-bill minibus focused on domestic spending, yet they have not start debating the second minibus, which contains the L-HHS spending measures. According to Politico, the debate was postponed by Senate Democrats who believe that the 302(b) allocation for the L-HHS bill is too low. NRHA would also like to see more robust funding, particularly for rural health priorities, in the Senate’s version of the L-HHS bill, but we understand that as the appropriations process is postponed, another Continuing Resolution is likely to be employed to ‘buy’ time. However, there is support from congressional leaders and the White House to have the appropriations bills finalized before the end of the year. So, even with the impeachment inquiry underway, we remain optimistic that progress will be made on passing/finalizing federal funding measures.
Health Care Provider Deserts May Leave Patients in the Cold
UNIVERSITY PARK, Pa. — People with health insurance under the Affordable Care Act (ACA) may have access to fewer health care providers — and may also have to drive further to see them — than people with other plans, according to researchers.
In a new study — published Nov. 4 as part of the November issue of Health Affairs — researchers found that people with ACA health insurance are more likely to find themselves in “artificial provider deserts,” areas where the health care providers near a customer are not covered by their insurance plan, leaving them without access to care even though providers are nearby.
Simon Haeder, assistant professor of public policy, said this is usually not a problem for people living in cities, but it can quickly become an issue for people living in more rural areas.
“If you’re of high socioeconomic status and relatively healthy, traveling long distances for care might be easier or not be a big issue for you,” Haeder said. “But if you’re more economically disadvantaged, and if you potentially don’t speak English or have multiple medical conditions, these challenges with provider networks can have large implications for your health.”
The researchers said that after the ACA was passed, there was a lot of research done on how ACA plans compared to commercial plans, like the ones people access through their employers. Haeder said that while this previous work found that ACA plans covered fewer providers and had lower premiums, researchers did not factor in how far people had to travel to see the health care providers covered by their insurance.
Read the entire press release here.
Appalachian Hospital Merger Exposes Tension over Rural Healthcare Access
Daily Yonder, Olivia Paschal
Regulators have put in place measures they hope will protect consumers in rural Central Appalachia from harm that might result from the merger of competing healthcare systems into a regional monopoly. Some community members are skeptical.
Commentary: How Rural Areas Can Avoid Being Undercounted in the Census
Daily Yonder, Amanda Gold and Yipeng Su
Will rural America gain population in the next Census? Part of that depends on how well rural people get counted. With billions of dollars and political representation on the line, rural places have a lot of reasons to prepare for the 2020 Census.
Legislation Seeks to Decrease Rural Maternal Deaths
Daily Yonder, Liz Carey
As pregnancy-related deaths in rural areas climb, federal lawmakers hope to reverse the trend with legislation that will attract more healthcare providers to rural areas and identify the causes of pregnancy-related deaths.
In September, U.S. Representative Xochitl Torres Small, D-New Mexico, introduced HB 4243, the Rural Maternal and Obstetric Modernization of Services Act (the Rural MOMS Act). The bill would add incentives to attract healthcare providers, fund equipment purchases, and support data collection on maternal health and morbidity in rural areas.
The U.S. ranks as one of the worst developed nations for maternal mortality, with more pregnancy-related deaths than Saudi Arabia and Kazakhstan. Rural parts of the U.S. have 60% higher mortality rates, according to 2015 data from the Centers for Disease Control (CDC). The report says the mortality rate in large central metropolitan areas was 18.2 per 100,000 live births, compared to 29.4 per 100,000 live births in the most rural areas.
In May, Seema Verna, the director of the Center for Medicare and Medicaid Services, said in her statement to the National Rural Health Association Conference in Atlanta that maternal health was one of her department’s top priorities.
“Maternal health is a growing concern in the country,” she said in her remarks. “About 700 women die each year in the U.S. due to pregnancy or delivery complications.” Nearly two-thirds of those deaths are preventable, she said.
Rural America’s higher maternal mortality rate “is particularly concerning to me… because early in my career, I worked on a healthy babies program and here we are… decades later… dealing with the same challenges… some of which have gotten worse,” Verna said. “Statistics show that pregnancy-related mortality deaths have almost doubled in the last 30 years.”
Since Verna’s speech in May, there’s been lots of discussion and fact finding, said Katy Backes Kozhimannil, director of the University of Minnesota Rural Health Research Center.
Click here to access the full article.


