- Miles for Milk: How Student-Run Grocery Store Reshaped Rural Community's Food Access
- Native Americans Have Shorter Life Spans, and It's Not Just Due to Lack of Health Care
- Promotoras Play Essential Role in Connecting Farmworkers with Health Care in Rural NorCal
- Using Medicaid to Address Young People's Mental Health Needs in School Settings
- Across the Country, Amish Populations Are on the Rise
- Sunsets, Wildlife and Limited Care: Challenges of Aging in Place in Rural America
- City-Country Mortality Gap Widens amid Persistent Holes in Rural Health Care Access
- Tribal Environmental Impact Network
- Minnesota's Rural Ambulance Providers Look to State Capitol for Their Own Lifeline
- Biden-Harris Administration Takes Action to Support the Primary Care Workforce
- Over 3,000 Homes on the Navajo Nation Receive Accurate Addresses for the First Time
- Rural Population Grows for Second Consecutive Year
- Rapides Library Offers Telehealth to a Town Without Doctors
- Rural Infection Preventionists Need Community Support
- New Federal Health IT Strategy Sets Sights on a Heathier, More Innovative, and More Equitable Health Care Experience
Pennsylvania DHS Releases Preliminary MATP Report
On October 28, 2019, the Pennsylvania Department of Human Services (DHS) released a preliminary report that reviews financial data, studies, and surveys related to the Medical Assistance Transportation Program (MATP) and non-emergency medical transportation brokerage programs. Per a legislative directive, DHS developed a MATP Analysis Workgroup to study the state’s shift to a brokerage model. The report outlines the data sources used as the foundation of the analysis and how the workgroup is seeking stakeholder feedback. The final analysis is scheduled for completion by December 28.
Pennsylvania Governor Wolf’s Administration Establishes Links for Continuity of Care for Pennsylvanians Reentering Their Communities
The Pennsylvania departments of Human Services (DHS) and Corrections (DOC) today announced that all of DOC’s state-run correctional facilities are connected to DHS’ Pennsylvania Patient & Provider Network (P3N). This marks a significant milestone in the commonwealth’s ability to help individuals to maintain continuity of their medical care before, during and after incarceration in a Pennsylvania state prison.
“DOC’s connection to the P3N will have a positive impact on health care for incarcerated and returning citizens by enabling the electronic sharing of information with thousands of health care providers connected to the five existing P3N certified Health Information Organizations (HIO) in Pennsylvania,” said DHS Secretary Teresa Miller. “This will bridge connections between care received while incarcerated to help returning citizens on their paths to healthy and productive lives.”
“Our charge every single day is to provide our inmate population with health care services that meet or exceed community standards,” said DOC Deputy Secretary for Administration Christopher Oppman. “Having immediate access to past medical records gives us the ability to provide timely, comprehensive care, which benefits the inmate and his/her health. Similarly, being able to provide critical information to outside health care providers upon release also ensures continuity of health care services and successful reentry back into the community.”
When an individual first enters an SCI, that facility will access that person’s medical data via the P3N to review the treatments and services they received from health care providers prior to their incarceration. This will give the correctional facility a better picture of a new inmate’s clinical history so that they can provide appropriate follow-up care while the person resides in that SCI.
Health care providers who are treating and caring for reentrants are also able to access vital information that providers should know when making clinical decisions. P3N network participants across the commonwealth will be able to access DOC’s patient information about treatments and services that individuals received during their periods of incarceration in a state correctional institution (SCI).
In addition to maintaining continuity of care, this bi-directional information exchange between DOC and the P3N also reduces the amount of time needed to access vital patient data and lowers costs by reducing duplicative tests and services.
Through this partnership with DHS, the DOC’s connection to the P3N gives SCI medical personnel the data needed to treat and serve new inmates. In addition, community health providers can better serve reentrants who have become their patients, helping them to achieve better health outcomes.
The P3N was established through Act 76 of 2016 to create a means of communication between health care providers, payers and patients. It creates efficiencies in health care delivery and promotes improved health outcomes for patients. The P3N links health information organization (HIO) member organizations to providers and payers across the state improving health care in their communities through increased coordination and communication between providers.
In July, Governor Tom Wolf signed an executive order strengthening protections for vulnerable populations such as re-entering citizens. As part of this effort, the administration is committed to supporting innovation in work and information sharing between agencies and our partners in the private sector. This expanded network of information sharing will help health care providers working in the SCIs and communities have more complete pictures of reentering citizens’ medical histories and do more to address their needs and barriers to good health.
For more information on the Department of Human Services, visit www.dhs.pa.gov.
For more information on the Department of Corrections, visit www.doc.pa.gov.
Pennsylvania Department of Transportation Published Draft Active Transportation Plan; Seeks Input
The Pennsylvania Department of Transportation (PennDOT) has published its Statewide Active Transportation Plan and is seeking public input. The plan identifies and prioritizes strategies that will promote more opportunities for bicyclists and pedestrians and promotes health and wellness activities that support objectives in the State Health Improvement Plan, especially strategies in the obesity, physical activity and nutrition focus. The plan includes information on developing and improving infrastructure that will support bicycling and pedestrian projects and enhance economic initiatives in rural and urban communities.
Public input is due by December 6, 2019 and should be submitted to ra-pdbikepedmsterpln@pa.gov.
Medicare Outpatient Payment Policies Finalized
On November 1, CMS finalized updates to the Medicare Outpatient Prospective Payment System (OPPS) and Ambulatory Surgical Care Center (ASC) Payment System for the 2020 calendar year. In addition to updating payment rates, this rule finalizes completing the two-year phase-in of site neutral payment for clinic visits when provided at an off-campus provider-based department. This final rule also finalizes to pay Average Sale Price (ASP) minus 22.5 percent for 340B-acquired drugs for CY 2020. Rural sole community hospitals are still exempted from the reduction and will continue to be paid ASP plus 6 percent. In the rule, CMS finalizes a change to the generally applicable minimum required level of supervision for hospital outpatient therapeutic services furnished by all hospitals and Critical Access Hospitals (CAHs) from direct supervision to general supervision. CMS is also finalizing for the OPPS, the other wage index policies adopted in the FY 2020 IPPS final rule. CMS plans to finalize these provisions on price transparency and requirements for making public a list of standard charges in a standalone document at a later date. As part of this rulemaking, CMS is accepting comments on the payment classifications assigned to the interim APC assignments and/or status indicators of new or replacement Level II HCPCS codes until 5 pm EST on December 2, 2019. Click here for more information from the Federal Register.
CMS Finalizes Medicare Clinician Policy, Payment, and Quality Provisions for CY 2020
On November 1, CMS issued a final rule that includes updates to payment policies, payment rates, and quality provisions for services furnished under the Medicare Physician Fee Schedule (PFS) effective on or after January 1, 2020. This includes three new telehealth codes to describe a bundled episode of care for treatment of opioid use disorders, Medicare coverage for opioid treatment programs, updates to care management services, implementation of a ground ambulance data collection system, and a revision to the current supervision requirement to clarify physician supervision requirements for physician assistants (PAs), among other updates. The rule also makes updates to Medicare’s Quality Payment Program including performance thresholds and category weights for the 2020 performance period and clarifying the definition of rural for the purposes of the Merit-Based Incentive Payment System (MIPS). As part of this rulemaking, CMS included an interim final rule with comment period (IFC) to establish coding and payment for evaluation and management, observation and the provision of self-administered Esketamine, with comments on that proposal due no later than 5 pm on December 31, 2019. Click here for more information from the Federal Register.
Deadline for Critical Access Hospitals to Submit a Hardship Exception Application – December 2
CMS requires that all Critical Access Hospitals (CAHs) use either the 2014 or 2015 Edition certified electronic health record technology (CEHRT) to meet the reporting requirements of the Medicare Promoting Interoperability Program and successfully demonstrate meaningful use. Downward payment adjustments must be applied to CAHs that are not meaningful users of CEHRT. However, CAHs may avoid the Medicare downward payment adjustments by completing a hardship exception application by December 2 to show that meeting the meaningful EHR user requirements would result in a significant hardship. Click here for more information.
AJPH Call for Papers on Rural Public Health –
The American Journal of Public Health (AJPH) invites papers assessing the role of government policy in the status and revitalization of rural health. They seek papers that describe rural health research, report on interventions in rural settings, assess the impact of laws and policies, and examine the human health impact of climate change in rural areas. AJPH also invites editorials and commentaries proposing ways to apply public health methods that have been successful in other regions of the world, describing potential sources of funding, and depicting a vision for a rural public health of the 21st century. Potential authors should visit the AJPH website to review instructions for authors and specific guidelines for the various types of manuscript formats. Abstracts are due on January 15, 2020.
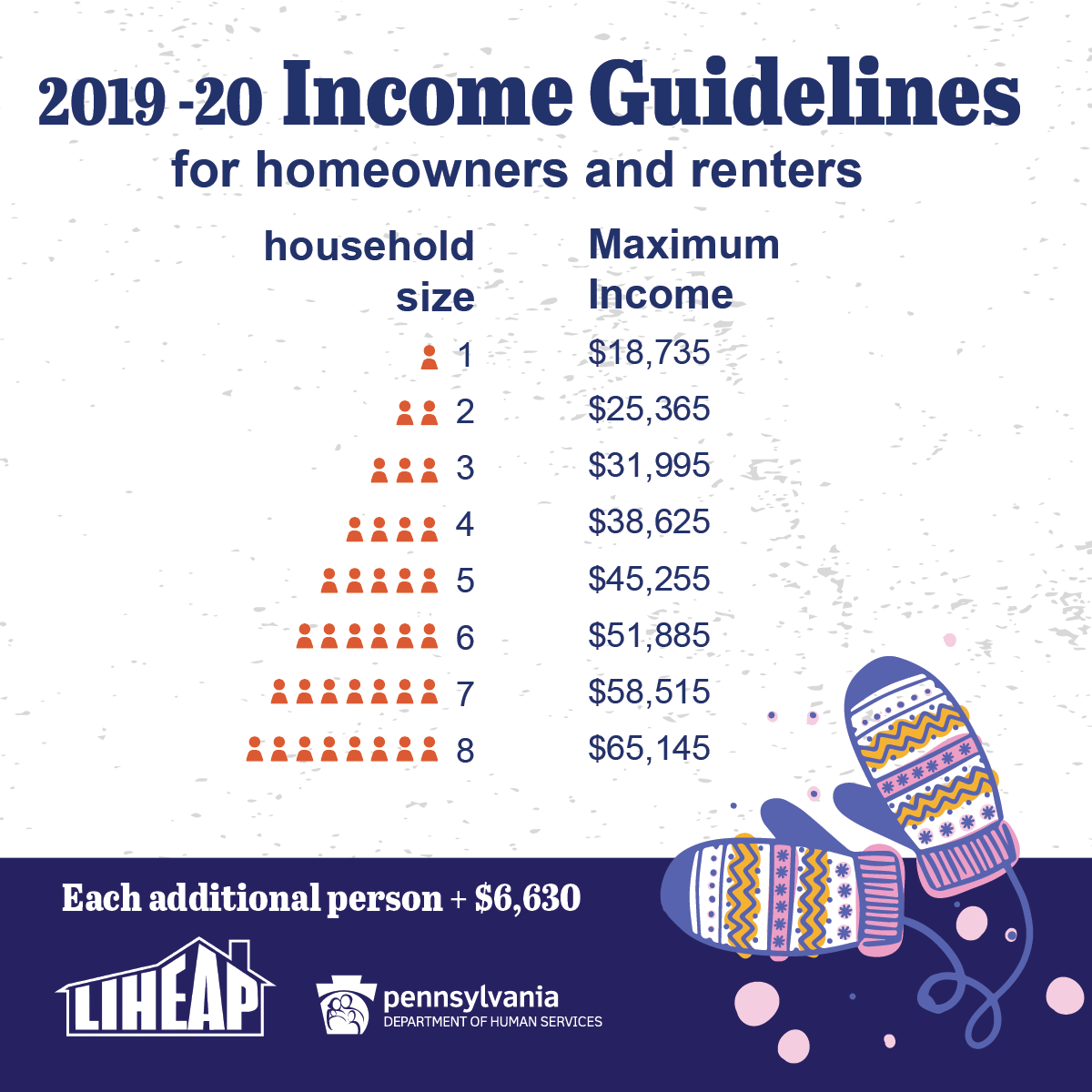
Home Heating Assistance is Now Available for Pennsylvania Families
LIHEAP, which stands for the Low-Income Home Energy Assistance Program, helps families living on low incomes pay their heating bills in the form of a cash grant. Crisis grants also are available for households in immediate danger of being without heat.
How cash grants work
A one-time payment is sent directly to the utility company/fuel provider and is credited on the heating bill. Cash grants range from $200 to $1,000 based on household size, income, heating region, and fuel type.
Qualifying crisis situations
- Broken heating equipment or leaking lines that must be fixed or replaced
- Lack of fuel
- Main heating source has been completely shut off
 Danger of being without fuel (less than 15-day supply)
Danger of being without fuel (less than 15-day supply) - Danger of having utility service terminated (received a notice that service will be shut off within the next 60 days)
Eligibility
- There are income guidelines.
- Applicants do not have to be on public assistance.
- Applicants don’t need to have an unpaid heating bill.
- Applicants can rent or own their home.
What’s needed to apply?
- Names of people in the household
- Dates of birth for all household members
- Social Security numbers for all household members
- Proof of income for all household members
- Recent heating bill or delivery receipt from the previous year
[For crisis situations, a person may need a copy of the shut-off notice.]
How to apply
Pennsylvanians can apply for LIHEAP three ways: online, on paper, and in person.
Online
Apply for LIHEAP benefits online using COMPASS. New this year: Those who received LIHEAP last year can apply for home-heating assistance via the mobile app, myCOMPASS PA. They’ll need the preseason application or green postcard we sent via mail to apply on the app.
On paper
Pennsylvanians can download an English or Spanish version of the application, fill it out, and return it to their county assistance office.
In person
Pennsylvanians can visit their county assistance office for help filling out the application in person. Applications also are available at senior centers and other community agencies.
Contact us for help
For more information about LIHEAP, Pennsylvanians can call the LIHEAP hotline at 1-866-857-7095, or can contact their county assistance office, Monday through Friday. Individuals with hearing impairments may call 711.
Visit the website
Find all of this information and more on the DHS website. View the state plan for LIHEAP and download brochures to print and share.
Forbes Explains How Urbanization Exacerbates the Health Care Crises in Rural America
Forbes reports that according to the USDA’s Economic Research Service, between 2010 and 2017, almost 1,000 rural counties in the U.S. recorded more deaths than births. Simultaneously, rural populations have declined, with only 20% of the population residing in rural areas which make up 97% of the country. Population change also means significant changes in health care need, demand and access. Also, according to the National Institute for Health Care Management (NIHCM), “As urbanization increases, an older, sicker and poorer population remains in rural America.” What this means is that Americans living in rural areas of the country have much greater health issues, and far fewer health resources.
Support for the Rural ACO Improvement Act Builds
The Rural ACO Improvement Act (S.2648) is gaining momentum on Capitol Hill. The recently introduced Senate bill would revise the Medicare Shared Savings Program benchmarking process and level the playing field for rural accountable care organizations. NRHA supports and applauds the legislation as a critical step to ensure all providers, regardless of zip code, are able to benefit from the program. We are proud that other associations with vested interested in the future of rural health care, such as AAFP, are joining us in supporting this meaningful rural health legislation.
