- Miles for Milk: How Student-Run Grocery Store Reshaped Rural Community's Food Access
- Native Americans Have Shorter Life Spans, and It's Not Just Due to Lack of Health Care
- Promotoras Play Essential Role in Connecting Farmworkers with Health Care in Rural NorCal
- Using Medicaid to Address Young People's Mental Health Needs in School Settings
- Across the Country, Amish Populations Are on the Rise
- Sunsets, Wildlife and Limited Care: Challenges of Aging in Place in Rural America
- City-Country Mortality Gap Widens amid Persistent Holes in Rural Health Care Access
- Tribal Environmental Impact Network
- Minnesota's Rural Ambulance Providers Look to State Capitol for Their Own Lifeline
- Biden-Harris Administration Takes Action to Support the Primary Care Workforce
- Over 3,000 Homes on the Navajo Nation Receive Accurate Addresses for the First Time
- Rural Population Grows for Second Consecutive Year
- Rapides Library Offers Telehealth to a Town Without Doctors
- Rural Infection Preventionists Need Community Support
- New Federal Health IT Strategy Sets Sights on a Heathier, More Innovative, and More Equitable Health Care Experience
Health Care Headlines, Business News & Trends
CDC Updates COVID-19 Masking and Monitoring Guidance
The Centers for Disease Control and Prevention (CDC) recently updated its framework to monitor the level of COVID-19 in communities. CDC leaders also announced that this data will inform recommendations on prevention measures like masking. They have updated their masks webpage to provide guidance based on the COVID-19 Community Level and personal risk factors. Read the full media briefing transcript.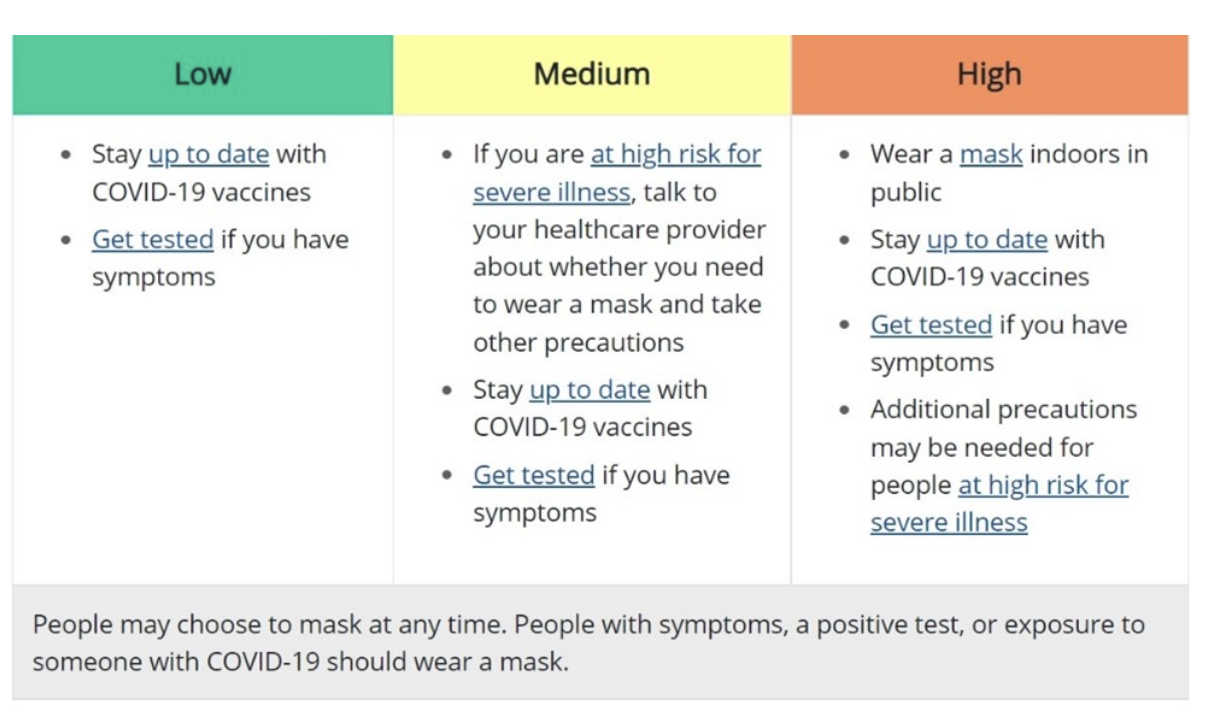
Race and Ethnicity Matter in Accessing Medical Care
The Medicaid and CHIP Payment and Access Commission (MACPAC) recently released an issue brief on Experiences in Accessing Medical Care by Race and Ethnicity. The brief uses data from the 2015-2018 National Health Interview Survey (NHIS) to assess Medicaid members’ access to care by race and ethnicity. Notably, the study found that Black, Hispanic, and Asian Medicaid members had significantly lower rates of receiving some preventive health screenings as compared to white non-Hispanic members and that Black and Hispanic Medicaid members were less likely than white non-Hispanic members to receive primary care and mental health care visits.
$88 Billion in Medical Debt on Consumer Credit Reports
Consumer credit reports contained $88 billion in medical debt as of June, a problem the federal agency that enforces financial protection rules vows to crack down on. Medical debt is far and away from the most common type of liability on credit reports. On Tuesday, Consumer Financial Protection Bureau (CFPB) officials questioned whether it belongs there at all. As of last year, 58% of all third-party debt collections were for medical debt, the agency determined in a new report. The CFPB found that about 20% of U.S. households owe a medical debt, which appears on 43 million credit reports.
Congress Turns Their Attention to Behavioral Health
In February, Senate and House Committees held a number of hearings on behavioral health, including two Senate Finance Committee hearings on youth mental health, a Senate HELP Committee hearing on mental health and substance use, a House Energy and Commerce Committee hearing on mental health, and two House Ways and Means Committee hearings on the mental health crisis, substance use, and suicide. Senate Finance Chair Wyden (D-OR) reportedly hopes to introduce a broad bipartisan package this summer focused on the integration of primary and mental health care, telehealth, parity, and children’s behavioral health.
Pennsylvania Governor Adds New Qualifying Life Event for Pennie Coverage
Gov. Tom Wolf this week announced that Pennsylvania’s state-based health insurance marketplace, Pennie, has added a new qualifying life event to allow low-income Pennsylvanians the ability to enroll in health insurance throughout the year. This new qualifying life event will allow Pennsylvanians with an annual household income equal to or below 150% of the federal poverty level to shop and enroll in health insurance through Pennie. Financial assistance, which nearly 90% of the almost 375,000 Pennie customers receive, is also available. Pennsylvanians enrolling during 2022 can also benefit from the increased subsidies provided by the American Rescue Plan, which has changed the affordability of health coverage across the nation.
To receive this new qualifying life event through Pennie, new customers will need to visit pennie.com, click “Get Covered” and apply. If the customer meets the income qualifications, a Special Enrollment Period will automatically open. Once the Special Enrollment Period opens, the customer will have 60-days to shop and enroll in a healthcare plan through Pennie. Currently, this opportunity is only available for those currently not receiving health coverage through Pennie. Beginning June 2022, existing Pennie customers whose income is lower than or equal to the 150% federal poverty level can update their application and change their current plan using this qualifying life event.
The Department of Veteran Affairs Creates a Graduate Medical Education & Residency Pilot Program

If finalized, a proposed rule from the U.S. Department of Veterans Affairs (VA) would place medical residents in existing or new residency programs and reimburse certain costs associated with graduate medical education. The VA is considering factors for determining clinical needs in certain areas, i.e., the ratio of veterans to VA providers, and for placement of residents in facilities outside of the VA. This will include an evaluation of the range of clinical specialties of VA and non-VA providers in underserved rural and tribal communities. A future request for proposal will announce opportunities for placement of residents at certain underserved VA facilities as well as certain Rural Health Clinics and Federally Qualified Health Centers. By statute, the pilot program prioritizes the placement of residents in Indian Health Service facilities, and Indian tribal or tribal organization facilities.
Pennsylvania Distributing No Cost OTC COVID-19 Rapid Tests for Vulnerable Populations
In order to close gaps in COVID-19 equity across the Commonwealth, the Pennsylvania Department of Health is providing OTC COVID-19 rapid tests at no cost to vulnerable populations across the Commonwealth and is seeking partners to help distribute tests in high-need communities. Partners can request tests via online form here: OTC Test Request Form. Any questions for the COVID-19 Testing Team should also be submitted using this form.
Participating organizations/entities must:
- Be able to receive delivery of and store tests on-site
- Determine test pickup times/dates, and local distribution strategy
- Communicate test availability to local vulnerable populations
Please note:
- Test quantity allocated is dependent on DOH’s supply on hand and submitting a request does not guarantee fulfillment
- Priority will be given to sites that can access high-need populations, e.g.,
- Areas with high social vulnerability index
- Limited COVID-19 testing alternatives
- Request fulfillment is limited to 2 requests per month
- For organizations that will broadly distribute to greater communities, we will periodically update the testing website (COVID-19 Testing | PA.GOV) to list location/time/dates for distribution
Social Vulnerability:
- Social vulnerability refers to the resilience of communities (the ability to survive and thrive) when confronted by external stresses on human health, stresses such as natural or human-caused disasters, or disease outbreaks. Reducing social vulnerability can decrease both human suffering and economic loss. Socially vulnerable populations include those who have special needs, such as, but not limited to, people without vehicles, people with disabilities, older adults, and people with limited English proficiency. The Social Vulnerability Index includes the following themes and social factors:
- Socioeconomic status (below poverty, unemployed, low/no income, no high school diploma)
- Household composition & disability (aged 65 or older, aged 17 or younger, older than age 5 with a disability, single-parent households)
- Minority status & language (minority, speak English “less than well”)
- Housing type & transportation (multi-unit structures, mobile homes, crowding, no vehicle, group quarters)
- Additional information from CDC on the Social Vulnerability Index can be found here: CDC/ATSDR SVI Frequently Asked Questions (FAQ) | Place and Health | ATSDR
National Strategy to Address Mental Health Crisis

Three strategy directives announced by the White House include: 1) Strengthen system capacity to expand the supply, diversity, and cultural competency of the mental health workforce, particularly in rural and underserved areas. This effort will include training and opportunities for paraprofessionals such as community health workers and peer recovery coaches. 2) Connect patients to care by expanding and strengthening access to mental health and recovery services. The President’s budget for fiscal year 2023 will propose that all health plans cover robust behavioral health services with an adequate network of providers, including three behavioral health visits each year without cost-sharing. 3) Create healthy environments by addressing social determinants of health. This will involve adjustment to standards and practices for online marketing and social media, expansion of early childhood and school-based intervention services, and mental health resources for incarcerated individuals. According to the 2020 results from the National Survey on Drug Use and Health, approximately 7.7 million nonmetropolitan adults reported having any mental illness, accounting for 20.5 percent of nonmetropolitan adults. At HRSA, our work to implement this strategy means taking action.
Health Experts Urge Against COVID-19 Complacency: 12 Calls to Action in New 136-page Plan
A team of 53 epidemiologists, pharmacologists, virologists, immunologists and policy experts published a 136-page report on the heels of the new COVID-19 preparedness plan released by the White House. Their plan shares similarities with that from the Biden administration but also differences, such as broadening the nation’s response to include all major respiratory viruses.
The group behind “A Roadmap for Living with COVID” is led by Ezekiel Emanuel, MD, PhD, vice provost for global initiatives at the University of Pennsylvania in Philadelphia and former advisory board member of the now-dissolved COVID-19 panel that guided President Joe Biden’s transition into office. The group includes former officials from both Republican and Democratic administrations. Find the complete listing of authors, contributors and reviewers here.
“The shift to the next normal should not induce complacency, inaction or premature triumphalism,” the authors note in their executive summary, which does not mention the Biden administration’s March 2 COVID-19 preparedness plan by name.
The roadmap is centered upon 12 calls to action:
1. Expand the focus of U.S. preparedness and response from COVID-19 to major respiratory viruses, including flu and RSV infection, with the interim goal to reduce annual deaths below the worst influenza season of the last decade.
2. Create, maintain and disseminate a transparent infectious disease dashboard to guide the public and policymakers at national, state and local levels on the introduction, modification and lifting of public health measures.
3. Strengthen testing, surveillance and data infrastructure. This includes production capacity for 1 billion at-home rapid tests per month, test-to-treat infrastructure that links testing to medical consults and treatment, and the establishment of infrastructure to rapidly collect and analyze data on population immunity.
4. Regulate the improvement and monitoring of indoor air quality. The group calls for the administration to direct the Environmental Protection Agency and Occupational Safety and Health Administration to create standards that protect workers from inhalation exposure.
5. Direct and fund HHS, including the NIH and FDA, to accelerate the development of new, more effective therapeutics, particularly multi-drug oral antivirals and next-generation vaccines that offer better, broader and longer-lasting protection. The authors want the administration to direct and fund HHS to achieve a vaccination rate of at least 85 percent by the end of 2022, which would include CMS reimbursing clinicians for discussing vaccinations with patients who are insured by Medicare and Medicare.
6. Shift the goal of U.S. contributions to the global vaccination effort from stopping infections through population vaccination coverage alone to improving the distribution and administration infrastructure necessary to fully vaccinate the most vulnerable.
7. Strengthen research on long COVID-19. The authors urge for coordinated and expanded research to answer questions on its frequency, risk factors, prognosis and benefits of vaccines and therapies for long COVID-19 within the next year, along with support for individuals experiencing the condition.
8. Create a permanent cadre of community health workers who will support populations highly susceptible to adverse outcomes from respiratory viruses.
9. Expand and support the healthcare workforce. Calls to action include greater pay, health benefits, tuition assistance, loan forgiveness and safe working conditions for workers. The group wants industrywide incentives to accelerate the adoption of automation for routine paperwork and chores, and the extension and expansion of temporary regulatory flexibilities that allowed healthcare organizations to operate telehealth and hospital-at-home programs throughout the pandemic.
10. Create a new post to fight biosecurity pandemic threats. The yet-to-be post, deputy assistant to the president for national security affairs and biosecurity, would sit within the National Security Council and be responsible for the preparation and response to any biosecurity and pandemic threats, including foreign and domestic sources of anti-science misinformation.
11. Redesign U.S. public health communications to regain public trust in a fast-moving, deeply polarized environment to promote the best health outcomes for Americans. The proposed redesign includes the creation of a Joint Information and Communication Center to oversee the sharing of infectious disease data, and infrastructure for dissemination of public health messages.
12. Roll out policies and programs to enable schools and child care facilities to remain open and safe for in-person learning and care without need for special public health mitigation measures. These measures include improved air filtration and expanded school nurse programs.
“Unfortunately, health crises in the United States are often followed by collective amnesia,” the authors contend, saying the roadmap is a plan for the United States to get to the next normal while building the systems and infrastructure needed to reduce risk of another pandemic and the consequences if one does occur.
Both “A Roadmap for Living with COVID” and the new COVID-19 preparedness plan released by the White House March 2 approach planning with a focus on living alongside the virus while continuing to combat it. The Biden administration’s 96-page plan is built around four goals: (1) protect against and treat COVID-19, (2) prepare for new variants, (3) prevent economic and educational shutdowns and (4) vaccinate the world. Read more about its contents here.
White House Moves to Identify ‘Disadvantaged’ Communities in Line for Federal Funding Boost
In a significant step toward changing how federal funds are distributed, the Biden administration has preliminarily identified nearly a third of the nation’s census tracts as “disadvantaged” and in line for more help from the federal government.
A week after taking office last year, Biden said he wanted to address historic inequities that have left disadvantaged communities around the country behind in receiving federal funding.
Federal agencies are still working through exactly how to do this. But in the meantime, the White House Council on Environmental Quality has provided a preliminary glimpse at which communities might benefit from Biden’s vision.
The first draft of the database identified 23,410 census tracts, or nearly a third of the nation, as disadvantaged. They represent a sweeping list of communities that could see more federal funds headed their way for climate change, clean energy and energy efficiency, clean transit, affordable and sustainable housing, training and workforce development, the remediation and reduction of legacy pollution, and the development of critical clean water infrastructure.
Among the communities described as “distressed” in the draft Climate and Economic Justice Screening Tool are big cities like Newark, New Jersey, but also rural areas like Mason County, Washington, which has seen a decline in the timber industry after protections were put in place decades ago to preserve the spotted owl.
To identify the areas, the administration considered a wide range of factors, from the expected loss of agriculture and population due to climate change, to traffic volume and diesel particulate exposure, to the cost of housing, to the rate of asthma, diabetes and heart disease in the community.
A solace for areas initially not considered distressed is that the database is a work in progress. Saying it wants to make sure it is not missing any communities in need, the environmental council posted a notice in the Federal Register, asking local and state government officials, academics and members of the public to examine the database and suggest ways to refine it by April 25.
“The hope is that the tool reflects the realities on the ground and we are properly identifying disadvantaged communities,” the council official said.
Particularly valuable will be national datasets that allow the government to compare communities around the country, the official said. But the council would also welcome local studies and data to further refine the tool.
Monica Lewis-Patrick, a member of a White House advisory committee and president and CEO of a Michigan water justice organization, We the People of Detroit, said she hoped relevant data not usually considered in federal funding decisions, like data gathered by community activists, will be included.
NRHA Offers Initial Statement on the Biden 2022 State of the Union Address

In the State of the Union Address, President Biden proposed his solutions to the biggest concerns we are currently facing as a nation, including those facing rural health.
The National Rural Health Association (NRHA) has been pleased to see a focus on rural communities early in the President’s term, recognizing that for too long rural communities have faced underinvestment and persistent poverty. Significant investments in rural through the American Rescue Plan and Bipartisan Infrastructure Package include addressing rural health coverage gaps, keeping rural hospitals open, addressing rural healthcare workforce shortages, as well as maintaining and expanding telehealth. These are in line with NRHA’s advocacy focus since the onset of the Biden Presidency.
Of note, the President used the speech to launch a new Strategy to Address our National Mental Health Crisis. Rural America suffers from the effects of long-standing shortages of specialty mental health services, long travel distances to obtain treatment, and stigma and cultural/ societal attitudes toward receiving behavioral health services. Last fall, NRHA provided comments to a Senate Finance Committee request for information on mental health care. Upon initial review of the President’s proposed mental health strategy, NRHA is pleased to see many of our recommendations reflected in this new initiative, especially around investing in a strong behavioral health workforce, integration of behavioral health and primary care, and addressing the opioid crisis. HHS Secretary Becerra will kick off the National Tour to Strengthen Mental Health to hear directly from Americans across the country about the behavioral health challenges they are facing and engage with local elected officials and leaders to strengthen the mental health and crisis care system in our communities.
Last night President Biden announced his proposals to address several issues important to rural areas, including:
- COVID-19 “test to treat” program which will allow individuals to receive antiviral pills on the spot when doing in person testing at local pharmacies and locations like community health centers and long-term care facilities.
- Addressing the cost of prescription drugs including Medicare drug negotiation.
- Continuing to advance maternal health care in America.
- Veterans health and addressing toxic exposure.
- Creating of ARPA-H, the Advance Research Projects Agency for Health.
Of potential concern, the President announced measures to improve nursing home quality, including minimum staffing levels and increased inspections. Given historic under-reimbursement by public payers and recent staffing shortages associated with COVID-19, NRHA is concerned about implications for rural nursing home facilities ability to meet the potentially burdensome new standards. NRHA will closely monitor developments and advocate on behalf of rural long-term care providers across the country.
NRHA supports the Administration’s Unity Agenda to bring together all parts of our country to address disparities among our citizens. NRHA looks forward to continuing work with the Administration and Congress to ensure that rural communities have access to critical health care they need and deserve.
In Deep Water? PA’s Water Assistance Program is Here to Help
Funding continues to be available for eligible individuals and families in Pennsylvania experiencing financial hardship due to the COVID-19 pandemic through the Low-Income Household Water Assistance Program (LIHWAP). This assistance can aid in maintaining households’ access to drinking and wastewater services essential to ongoing health and overall wellbeing.
Program funds are issued directly to the service providers in the form of grants, or crisis grants depending on situation severity. To qualify for the program, participants must either rent or own their home, have overdue water bills, and meet program income guidelines.
The Department of Human Services (DHS) developed a media toolkit to assist in the awareness of the Water Assistance program within the commonwealth. Below are example social media posts. Additional social media images, newsletter text, and flyer text are available on the DHS website. Click here to apply!

